Abstract
Introduction HCT is the only therapy for SCD with curative intent, but the alkylator chemotherapies used in preparative regimens place patients at high risk for gonadal dysfunction. Adequate ovarian and testicular hormone production post-HCT is important for optimal health.
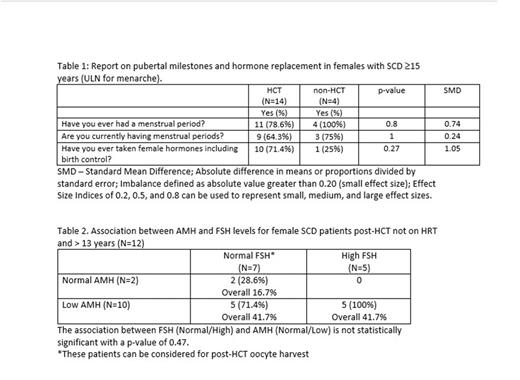
Methods We enrolled children and adults with SCD ≥ 1-year post-HCT ("HCT") in the Sickle Cell Transplant Evaluation of Long-term and Late Effects Registry (STELLAR) and a control group of patients with SCD not treated with HCT ("non-HCT"). We obtained annual surveys of gonadal health using a web-based platform. Surveys were completed by proxies for individuals <18 years and were self-report for individuals ≥18 years. Markers of ovarian reserve or testicular function were measured, including follicle-stimulating hormone (FSH) and anti-Müllerian hormone (AMH) in females and FSH and testosterone in males. The most recent survey was used for analysis when multiple surveys were available. The upper limit of normal (ULN) for age of pubertal onset was defined as 13 years in females and 14 in males, and the ULN for menarche was 15 years. Only females >13 years and males >14 years (ULN for activation of the hypothalamic pituitary gonadal axis) were included in the FSH analysis. Descriptive statistics were reported as median (Interquartile range [IQR]: 3rd quartile - 1st quartile), mean (min, max) or count (%). Statistical procedures involved a chi-squared test. The effect size was calculated using standard mean difference (SMD).
Results Surveys were completed by 48 SCD HCT patients (30 females, 18 males) and 12 SCD control patients (8 females, 4 males). Median age (IQR) at survey completion was 14.8 years (11.8) for female HCT, 16.0 (10.4) for male HCT, 14.5 (11.6) for female non-HCT, and 21.0 (22.8) for male non-HCT. Median age (IQR) at HCT was 8.8 years (6.1) for females and 9.1 years (5.2) for males. Most patients underwent HCT in 2010-2020 (86.7% of females, 78.8% of males). Donor was predominantly matched related (90.0% of females, 94.4% of males) with bone marrow stem cell source (90.0% of females, 94.4% of males). Most patients received myeloablative conditioning (86.7% of females, 94.4% of males). Only female HCT patients (n=8, 32%) reported being told they might need hormones to enter puberty. In females who were ≥15 years, menarche was reported in 11 (78.6%) HCT and all of the non-HCT patients. Current menstruation was reported in 9 (64.3%) HCT and 3 (75.0%) of non-HCT patients, and 10 (71.4%) HCT and 1 (25%) non-HCT females reported ever having taken hormones, including birth control. P-values and SMD can be seen in Table 1. Hormone levels were measured in 68 HCT patients (41 female, 27 male). Most patients underwent HCT from 2010-2020 (82.9% of females; 74.1% of males) using matched related donor (90.2% of females, 92.6% of males) bone marrow (87.8% of females, 85.2% of males) following myeloablative conditioning (87.8% of females, 88.9% of males). For females, the median age at the time of AMH testing was 16.5 years (IQR 9.1) with a mean of 6.8 years (IQR 4.8) post-HCT. Based on the age and assay normal values, AMH levels were normal in 3 (7.3%), low but detectable in 7 (17.1%), and undetectable in 31 (75.6%) of patients. FSH was measured in 12 females who were >13 years and not on hormone therapy (Table 2). The median age at FSH testing was 18.0 years (IQR 5.1), with a mean of 8.7 years (IQR 3.5) post-HCT. FSH levels were normal in 7 (58.3%) and above the ULN in 5 (41.7%), 3 of which were menopausal (>30mIU/mL). Testosterone values were obtained in 15 males who were >14 years with a median age 18.9 years (IQR 5.9) and a mean of 6.9 years (IQR 5.1) post-HCT. The mean testosterone level was 365.8 ng/dl (range 152-592), 13 (86.7%) of which were in the normal range and 2 (13.3%) being low. FSH values in males >14 years were high in 4 (26.7%).
Conclusions Nearly all females had diminished ovarian reserve post-HCT, with >75% having undetectable AMH levels. In addition, close to half of the females had elevated FSH levels, some in the menopausal range. However, females with normal FSH and normal or low AMH can consider post-HCT mature oocyte cryopreservation. Most males had normal testosterone levels, but >25% had elevated FSH levels which could be a signal of impaired spermatogenesis. These findings highlight the importance of studying the impact of HCT on gonadal function and the consideration of these outcomes when developing protocols for curative therapy in SCD.
Disclosures
Guilcher:Bluebirdbio: Other: PI of Project Sickle Cure, a Sickle Cell Transplant Advocacy and Research Alliance study partially funded by bluebirdbio. Bhatia:Columbia University Irving Medical Center: Membership on an entity's Board of Directors or advisory committees; Vertex Pharmaceuticals: Membership on an entity's Board of Directors or advisory committees, Other: Support for attending meetings and/or travel, Speakers Bureau. Gomez-Lobo:NICHD: Other: Funded by grant Z1A HD008985.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal